A tooth abscess is a painful infection that forms when bacteria invade the inner layers of your tooth or gum tissue. It usually starts as a simple cavity or gum irritation, but if left untreated, it can develop into a pocket of pus filled with harmful bacteria. This pus buildup causes pressure, inflammation, and sharp or throbbing pain that can radiate to the jaw, ear, or neck.
Understanding the stages of a tooth abscess is crucial because the infection doesn’t appear overnight—it progresses. At first, you might notice only mild sensitivity or discomfort, but as bacteria spread deeper into the tooth, the pain intensifies and swelling may occur. Without proper treatment, the infection can eventually reach the bloodstream, leading to serious health complications.
Common symptoms to watch for include persistent toothache, gum swelling, bad breath, pus drainage, and a bitter taste in the mouth. Some people also experience fever or swollen lymph nodes, especially if the infection spreads. The earlier you identify these signs, the easier it is for your dentist to stop the infection before it causes long-term damage.
In short, a tooth abscess isn’t something to ignore. Recognizing its early stages can mean the difference between a simple treatment and a dental emergency.
What Is a Tooth Abscess?
A tooth abscess is a pocket of pus that forms inside the mouth due to a bacterial infection. It usually develops when harmful bacteria invade the soft tissues of the tooth or gums, often through a crack, cavity, or untreated decay. When the body detects infection, it sends white blood cells to fight it off, creating pus—a thick fluid made of bacteria, tissue debris, and immune cells.
If the infection isn’t treated early, this pus has nowhere to go, leading to swelling, pressure, and intense pain. Over time, the abscess can spread deeper into surrounding tissues, affecting your jawbone and even causing swelling in the face or neck.
Types of Tooth Abscesses
Not all abscesses are the same. Understanding their differences helps you recognize where the infection starts and how it spreads:
- Periapical Abscess:
This type begins in the tooth’s pulp—the soft center that contains nerves and blood vessels. It’s usually caused by deep decay or trauma that allows bacteria to reach the pulp. Pain is often severe and may radiate to nearby areas. - Periodontal Abscess:
Found in the gums or bone surrounding a tooth, this abscess typically develops from advanced gum disease (periodontitis). You might notice gum swelling, bleeding, or a bad taste from pus draining through the gumline. - Gingival Abscess:
A more surface-level infection, often caused by trapped food particles or foreign objects like popcorn shells. Though minor compared to other types, it can still cause redness, pain, and tenderness.
Why Does a Tooth Abscess Form?
The root cause is almost always bacteria—but several factors can trigger it:
- Untreated cavities that reach the tooth pulp.
- Gum disease that exposes deeper tissues to bacteria.
- Cracked or broken teeth that allow bacteria to enter.
- Poor oral hygiene and plaque buildup.
In short, a tooth abscess is your body’s alarm signal that something is seriously wrong. Recognizing where and why it forms is the first step to getting it treated before the infection spreads further.
The 5 Stages of a Tooth Abscess
A tooth abscess doesn’t happen overnight—it’s a progressive infection that worsens with time. Understanding these five stages helps you spot the warning signs early, get timely treatment, and prevent serious complications. Let’s break down what happens at each stage.
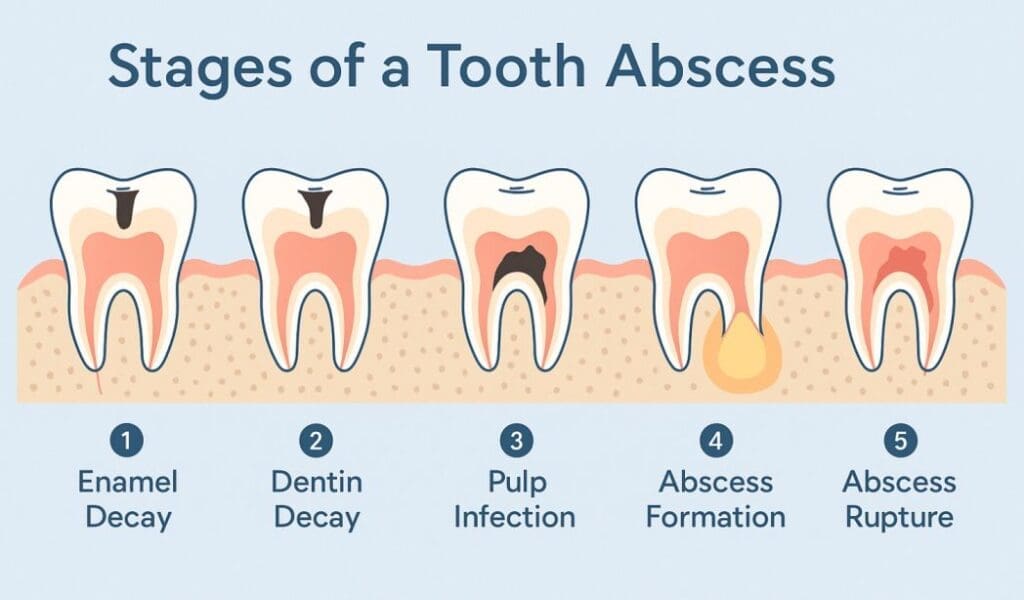
Stage 1: Enamel Decay
This is the starting point of most abscesses. Bacteria in plaque begin attacking the tooth’s outer layer (enamel), creating tiny holes or weak spots. At this stage, symptoms are subtle—maybe a bit of sensitivity when you eat something hot, cold, or sweet. Most people overlook it because it’s not painful yet, but this is when preventive care (like a filling) can stop the problem from progressing.
Stage 2: Dentin Decay and Infection Spread
Once bacteria break through the enamel, they reach the dentin, the softer layer beneath. This part has small tubules that lead directly to the tooth’s nerve, making it more vulnerable. You may start to notice a persistent toothache, mild swelling around the gumline, or discomfort when biting. The infection is now spreading deeper inside the tooth and getting harder to reverse without professional care.
Stage 3: Pulp Infection (Pulpitis)
Now the bacteria have reached the pulp, the inner core of your tooth containing nerves and blood vessels. This stage is where pain becomes severe and throbbing. The tooth may become extremely sensitive to heat, cold, and pressure. You might even have difficulty sleeping because the ache worsens when lying down. At this point, the infection is alive and active, and treatment like a root canal is often required to remove the infected tissue.
Stage 4: Abscess Formation
If the infection is left untreated, it moves beyond the tooth and forms a pocket of pus—the abscess itself. This can occur at the tooth root or in the surrounding gum tissue. The swelling becomes noticeable, and you might experience a bad taste in your mouth as the abscess starts draining. Fever, tender lymph nodes, and jaw pain are also common. Sometimes, a small bump (called a gum boil) appears near the affected area, which is a visible sign of the abscess.
Stage 5: Abscess Rupture or Spread
In the final and most dangerous stage, the abscess may rupture, releasing pus and giving temporary relief. However, this doesn’t mean the infection is gone—bacteria can now spread to the jaw, face, or even bloodstream, leading to severe complications like sepsis. This is a dental emergency that requires immediate professional attention.
Each stage of a tooth abscess builds on the last, and waiting too long to act only makes treatment more complex. Early detection and prompt dental care can save your tooth—and protect your overall health.
Common Symptoms Throughout the Stages
No matter which stage a tooth abscess is in, certain warning signs tend to show up along the way. Paying attention to these early symptoms can help you take action before the infection gets serious.
- Persistent or Sharp Toothache
A toothache that doesn’t go away is one of the clearest signs of an abscess forming. At first, it may feel like mild discomfort when chewing or biting, but over time it becomes a constant, throbbing pain that can radiate to your ear, jaw, or neck. This pain often worsens at night or when you lie down, because of increased pressure in the infected area.
- Gum Swelling or Redness
As the infection spreads, it triggers inflammation in the gums. You may notice puffiness, tenderness, or redness around the affected tooth. In more advanced stages, a small bump or boil filled with pus may form on the gum line. This is your body’s way of trying to drain the infection—but it’s also a sign that the abscess is progressing.
- Sensitivity to Pressure and Temperature
A developing abscess can make your tooth hypersensitive to temperature changes and pressure. Drinking cold water, eating hot soup, or even brushing your teeth might cause discomfort. This happens because the infection irritates the tooth’s nerve endings and increases inflammation around the root.
- Pus Discharge or Bad Breath
When pus begins to drain from the abscess, you might notice a foul taste or bad smell in your mouth. Persistent bad breath (halitosis) can also indicate that bacteria are actively multiplying in the infected area. While this might bring temporary relief from pressure, it’s a clear sign that the infection is still present and needs treatment.
- Fever, Swollen Lymph Nodes, or Fatigue
In severe cases, the body starts reacting to the infection as it spreads beyond the tooth. You may develop a fever, feel unusually tired, or notice swollen lymph nodes near your jaw or neck. These are signs that the infection is entering your bloodstream—a stage that requires immediate dental or medical attention.
Even if symptoms seem minor, a tooth abscess never heals on its own. If you notice any of these red flags, it’s best to contact your dentist right away. The sooner the infection is treated, the easier and less painful your recovery will be.
How Long Does a Tooth Abscess Take to Form?
A tooth abscess doesn’t appear overnight — it’s the result of a gradual process that can take anywhere from a few weeks to several months, depending on how fast bacteria spread and how your body responds. What begins as a small cavity or gum irritation can slowly evolve into a painful, pus-filled infection if left untreated.
From Cavity to Infection
At first, a small cavity may form in the enamel, often without any pain. Over time, as bacteria eat through the enamel and reach the dentin, the decay deepens and moves closer to the tooth pulp. Once bacteria invade the pulp — the soft tissue containing nerves and blood vessels — the infection can spread quickly, causing swelling and pressure inside the tooth.
If the infection continues unchecked, it extends beyond the root into the surrounding gum or bone, forming an abscess. For some, this may happen within a few weeks if decay is severe, while in others, it may take months to fully develop.
Factors That Speed Up Abscess Formation
Several conditions can accelerate how quickly a tooth abscess develops:
- Poor oral hygiene: Skipping brushing or flossing allows plaque and bacteria to build up faster.
- Untreated cavities or cracks: These create direct pathways for bacteria to reach deeper layers of the tooth.
- Weakened immune system: People with diabetes, autoimmune disorders, or chronic illnesses are more vulnerable to infections.
- Gum disease: Periodontal pockets provide ideal hiding spots for bacteria to multiply.
- High sugar diet: Frequent sugar intake feeds harmful bacteria, speeding up decay.
Why Timing Matters
Even though an abscess might take weeks or months to fully form, it’s important not to wait until pain becomes unbearable. Early intervention—like treating a cavity or mild infection—can prevent a full-blown abscess and save the natural tooth.
The takeaway? A tooth abscess develops slowly, but the damage it causes can escalate fast. If you notice even mild tooth pain or sensitivity, getting it checked early is the best way to avoid serious complications later.
Treatment Options for a Tooth Abscess
When it comes to treating a tooth abscess, time is everything. The goal is to eliminate the infection, relieve pain, and prevent the bacteria from spreading to other parts of the body. Depending on the severity of your abscess and where it’s located, your dentist may recommend one or more of the following treatments.
Draining the Abscess
The first step in treating a severe abscess often involves draining the pus to relieve pressure and pain. Your dentist will make a small incision in the swollen area and allow the infected fluid to escape. This instantly reduces discomfort, but drainage alone isn’t a cure — the underlying infection must still be treated to prevent it from returning.
Root Canal Therapy
If the infection has reached the tooth pulp, a root canal is usually the most effective way to save the tooth. During this procedure, the dentist removes the infected tissue, cleans out the canals, disinfects them, and then seals the space with a filling or crown. Root canals not only stop the infection but also preserve the natural tooth, preventing the need for extraction.
Tooth Extraction
In cases where the abscessed tooth is too damaged to repair, extraction may be necessary. Removing the infected tooth stops the bacteria from spreading further into the jaw or bloodstream. After extraction, your dentist may discuss options for replacement, such as a dental implant or bridge, to maintain your bite and appearance.
Antibiotics for Infection Control
If the infection has spread beyond the immediate area of the tooth or if swelling is severe, your dentist may prescribe antibiotics. These medications help control the bacterial spread and support your body’s healing process. It’s important to finish the full course of antibiotics, even if you start feeling better, to ensure the infection is completely cleared.
Pain Relief and Home Care Tips
After treatment, managing pain and promoting healing are key. Your dentist may suggest:
• Taking over-the-counter pain relievers like ibuprofen.
• Rinsing with warm salt water to reduce inflammation and promote healing.
• Avoiding hard, hot, or spicy foods that can irritate the area.
• Maintaining good oral hygiene—brushing gently and keeping the area clean.
Treating a tooth abscess isn’t just about relieving pain—it’s about stopping the infection at its source and preventing future issues. With timely dental care and proper aftercare, most patients recover quickly and fully. The sooner you act, the easier it is to save your tooth and restore your oral health.
Healing and Recovery Stages After Treatment
Once your tooth abscess has been treated—whether through drainage, a root canal, or extraction—the healing process begins. Recovery is usually smooth and straightforward, but understanding what to expect can help you manage discomfort and prevent future infections.
What to Expect After Treatment
Immediately after treatment, you might notice mild soreness or tenderness around the treated area. This is normal and typically lasts for a few days. If your dentist performed drainage, there may be a small open area in the gums that heals on its own. For root canal patients, the tooth may feel slightly sensitive to pressure while the tissues around the root recover.
You might also experience minor swelling or discomfort when eating, but this gradually improves. Applying a cold compress and using over-the-counter pain medication (like ibuprofen or acetaminophen) can help ease any post-procedure pain.
Healing Timeline
Most patients fully recover from a tooth abscess within 1 to 2 weeks, though this depends on the treatment method and the severity of the infection.
- After drainage: Recovery often takes just a few days once the infection pressure is released.
- After a root canal: You may feel soreness for about 5–7 days, but normal activities can usually resume immediately.
- After extraction: Healing takes slightly longer, typically up to two weeks, as the gum and bone rebuild around the empty socket.
If antibiotics were prescribed, continue taking them exactly as directed, even if symptoms disappear early. This ensures the infection is completely eliminated and doesn’t return.
Tips for Faster Recovery
Speeding up recovery and keeping your mouth healthy after an abscess treatment is all about gentle care and prevention.
- Maintain good oral hygiene: Brush and floss gently around the treated area to prevent bacteria buildup.
- Avoid hard or crunchy foods: Stick to soft foods for a few days to reduce irritation.
- Rinse with warm salt water: It helps cleanse the area and promote healing.
- Stay hydrated: Water helps flush out toxins and maintain saliva flow, which naturally fights bacteria.
- Follow up with your dentist: Attend your post-treatment appointments to ensure healing is on track.
Recovery from a tooth abscess is generally quick when you follow your dentist’s instructions. Within days, most people experience relief from pain and swelling—and within weeks, the treated area feels completely normal again. By maintaining good dental hygiene and getting regular check-ups, you can prevent abscesses from returning and keep your smile healthy for the long run.
Risks of Ignoring a Tooth Abscess
A tooth abscess is not just a dental problem—it’s a serious infection that can have far-reaching effects if left untreated. Many people make the mistake of waiting for the pain to “go away on its own,” but what’s really happening is the infection spreading deeper beneath the surface. Ignoring an abscess can turn a small, treatable issue into a major medical emergency.
1. Infection Spreading to the Jawbone and Surrounding Areas
When a tooth abscess is not treated promptly, the bacteria can spread from the root of the tooth into the jawbone, facial tissue, and even the sinuses. This condition, known as osteomyelitis (jawbone infection), can cause severe swelling, pain, and difficulty opening the mouth or chewing. In some cases, the infection can create new abscesses in nearby tissues, complicating treatment and recovery.
2. Sinus Infections and Facial Swelling
An upper-tooth abscess can sometimes extend into the maxillary sinuses, leading to a painful sinus infection. You might feel pressure or fullness around your cheeks and eyes, and chronic sinus issues can develop if the dental source isn’t treated. Facial swelling caused by an untreated abscess can also restrict movement and distort facial appearance, making even speaking or swallowing difficult.
3. Sepsis and Life-Threatening Complications
If the bacteria from a tooth abscess enter your bloodstream, it can trigger a condition called sepsis—a life-threatening infection that affects the entire body. Symptoms include high fever, rapid heart rate, and confusion. Sepsis requires immediate hospitalization and intensive medical care. Though rare, this outcome highlights how dangerous a seemingly “small” dental infection can become if ignored.
4. Tooth Loss and Bone Damage
A prolonged abscess can destroy the tooth’s root, surrounding bone, and gum tissue, making it impossible to save the tooth. Once the infection eats away at these structures, tooth loss becomes inevitable. Additionally, bone loss in the jaw can affect the stability of nearby teeth and limit future treatment options, like implants or bridges.
5. Chronic Pain and Long-Term Oral Issues
Even if the abscess drains on its own, the infection doesn’t disappear completely. The bacteria remain active and can cause recurring pain, inflammation, and foul taste in the mouth. Chronic abscesses can weaken your immune system and contribute to ongoing dental and systemic health issues.
Ignoring a tooth abscess is like letting a small fire burn unchecked—it will only grow and spread. Early treatment not only saves your tooth but also protects your overall health from serious complications. If you ever experience persistent tooth pain, swelling, or pus, don’t wait—see a dentist right away.
How to Prevent a Tooth Abscess
The best way to deal with a tooth abscess is to stop it from forming in the first place. Prevention is all about building daily habits that keep bacteria under control and catching small dental problems before they turn into painful infections. With a few simple but consistent steps, you can protect your teeth, gums, and overall oral health.
1. Brush and Floss Every Day
The foundation of abscess prevention starts with good oral hygiene. Brush your teeth twice a day using a fluoride toothpaste to remove plaque—the sticky film that harbors bacteria responsible for decay. Don’t forget to floss daily, as bacteria often hide between teeth where your toothbrush can’t reach. This simple routine can drastically reduce your risk of cavities and gum infections that lead to abscesses.
Pro tip: Replace your toothbrush every 3 months, or sooner if the bristles start fraying. A worn-out brush can’t clean your teeth effectively.
2. Don’t Skip Dental Checkups
Regular dental visits aren’t just about cleanings—they’re your early warning system against infection. Your dentist can spot cavities, cracks, or gum issues before they become painful abscesses. Aim to schedule a checkup every six months, or more often if you have a history of dental problems. Early treatment for even the smallest cavity can prevent major complications later.
3. Treat Cavities and Gum Problems Early
One of the leading causes of abscesses is untreated decay or gum disease. If you notice tooth pain, swelling, bleeding gums, or sensitivity, don’t ignore it. Getting a small cavity filled or treating gingivitis early can stop bacteria from spreading to the inner layers of your tooth. The longer you wait, the greater the risk of infection reaching the root.
4. Eat a Tooth-Friendly Diet
Your diet plays a huge role in your oral health. Limit sugary and acidic foods like soda, candy, and citrus drinks—they feed the bacteria that cause decay. Instead, include calcium-rich foods (like milk, cheese, and leafy greens) and vitamin C–rich fruits that support healthy gums. Drinking plenty of water also helps wash away food particles and maintain saliva flow, your mouth’s natural defense against bacteria.
5. Protect Your Teeth from Damage
Cracked or chipped teeth create openings for bacteria to enter. If you grind your teeth at night, consider wearing a mouthguard, and always wear one during contact sports. Small fractures can quickly turn into deep infections if left untreated.
Preventing a tooth abscess isn’t complicated—it’s about consistency and awareness. By brushing, flossing, eating smart, and visiting your dentist regularly, you can keep your teeth strong and infection-free. Remember, early action is the best protection against pain, swelling, and costly dental treatments down the line.
FAQs About Tooth Abscesses
Tooth abscesses can be painful, confusing, and sometimes even scary if you’re unsure what’s happening inside your mouth. Here are answers to some of the most common questions people ask about abscesses—so you can understand what to expect and when to seek help.
How Do I Know If I Have a Tooth Abscess?
A tooth abscess often starts with a persistent, throbbing pain that doesn’t go away. You might also notice swelling in your gums or face, sensitivity to heat or cold, and sometimes a bad taste in your mouth caused by pus. In more advanced stages, you may even see a small bump on your gums, called a “gum boil,” which indicates pus buildup.
If your pain becomes severe or spreads to your jaw, ear, or neck, it’s a sign the infection is getting worse—and you should see a dentist immediately.
Can a Tooth Abscess Heal Without Antibiotics?
Unfortunately, no—a tooth abscess cannot heal on its own. While the pain might fade temporarily if the abscess drains, the underlying infection remains and can quickly return. Antibiotics can help control the infection, but they don’t remove the source (like infected pulp or decay).
The only way to fully treat an abscess is through professional dental care, such as drainage, a root canal, or in severe cases, tooth extraction. Think of antibiotics as temporary relief, not a cure.
What Happens If an Abscess Bursts on Its Own?
If your abscess bursts, you may notice a sudden rush of foul-tasting fluid in your mouth and a temporary drop in pain. However, this doesn’t mean the infection is gone. The bacteria are still present and can spread deeper into the jaw or bloodstream.
Even if the swelling goes down, you should still see your dentist as soon as possible. They’ll clean the area, drain any remaining pus, and ensure the infection doesn’t return or worsen.
Is a Tooth Abscess an Emergency?
Yes, a tooth abscess is considered a dental emergency—especially if you have swelling in your face or neck, fever, or difficulty breathing or swallowing. These are signs that the infection may have spread beyond your tooth. Immediate dental treatment can prevent serious complications like sepsis or bone infections.
If your dentist isn’t available and your symptoms are severe, go to the emergency room for immediate care.
How Long Does It Take for Swelling to Go Down After Treatment?
After treatment—whether it’s a root canal, drainage, or extraction—swelling typically begins to reduce within 48 to 72 hours. Complete healing may take one to two weeks, depending on the severity of the abscess and your overall health.
To speed up recovery:
- Take prescribed antibiotics as directed.
- Rinse with warm salt water to reduce inflammation.
- Use cold compresses for swelling.
- Avoid hard or hot foods for a few days.
If the swelling or pain worsens after a few days, contact your dentist. It could mean the infection hasn’t fully cleared.
Understanding these FAQs can help you take the right steps early and avoid the serious risks of untreated dental infections. Remember, even a small abscess can become dangerous if ignored—so if something feels off, don’t wait. A quick dental visit today can save you from major complications tomorrow.
